Hypoglycemia is the presence of low blood sugar. Most people have heard the word hypoglycemia associated with those who are unable to go long periods of time without eating, or individuals with Diabetes. While these conditions do present life-threatening moments of hypoglycemia, there are other critical conditions where hypoglycemia occurs.
Digestive Patterns
When a person eats, the body begins to digest food upon its entrance to the stomach. The gastric juices and acids churn food particles into smaller pieces by muscle contractions called Peristalsis. This complete process takes around four hours. Food begins leaving the stomach before the final pieces are churned. The churned mixture is called chyme. Chyme leaves the stomach through contractions of the pylorus. The pylorus is the muscle at the bottom of the stomach whose sole purpose is to regulate the passage of chyme into the small intestines. It is a sphincter muscle that relaxes as needed, and remains contracted when not in use.
The sphincter muscle is supposed to release chyme in rhythmic patterns. Certain medical conditions can cause these patterns to speed up, slow down, or stop altogether. Post-Prandial Hypoglycemia (PPH) occurs when the pyloric sphincter releases too much chyme at once into the small intestines. The first third of the small intestines receiving the chyme is called the duodenum. PPH is also called “Dumping Syndrome,” or Reactive Hypoglycemia. It is defined as “symptomatic hypoglycemia occurring within four hours after a high carbohydrate meal in people who do not have Diabetes.”
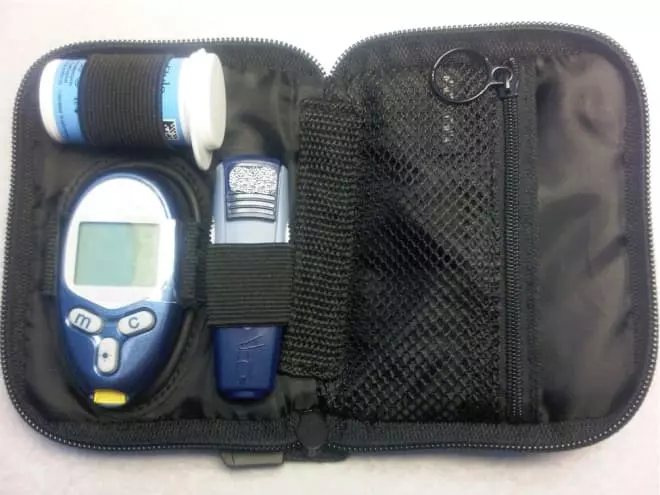
Photo Credit: by Katie R
Chyme is a mixture of small amino acids and sugar particles known as saccharides. As chyme moves into the small intestines, the blood stream takes up a large amount of a monosaccharide called glucose. Glucose is the body’s key source of energy. Glucose fuels the organs and tissues and produces energy through a process known as the Citric Acid Cycle. Blood sugar is a term that refers to the amount of glucose in the bloodstream at any present time. Ideal fasting blood sugar levels range between 70-100 for the normal full grown adult. Once you’ve eaten a meal, normal blood sugar levels increase to approximately 170-200. Hours after eating, those numbers drop into the low to mid 100s and continue dropping until they reach normal fasting levels.
The pancreas watches very closely as the glucose is absorbed into the blood stream. When the bloodstream has enough glucose, the pancreas releases insulin. Insulin is a hormone that helps your body use glucose for energy. It’s other function is storing excess glucose in the liver in the form of glycogen, a process called Glycogenesis. As glucose levels continue to rise, the pancreas secretes more insulin to signal the uptake of glucose into the liver. Glucose continues to be stored in the liver as long as it is present in the blood and the pancreas continues releasing insulin.
After eating, the body begins using glucose as energy. As glucose levels drop, the body begins using the stored glycogen. Glycogen is broken down in the liver through a process known as Glycolysis. The glucose produced is then able to be used as energy for the body’s cells. Hypoglycemia occurs when glucose levels drop to unsafe levels and glycogen is not able to keep up. Blood sugar levels below 70 are typically consider unsafe. Each individual has varying degrees of normal vs abnormal blood sugar. For most of us, glucose measurements in the 60 are a warning we need to eat something.
Gastric Dumping
Sometimes food moves too quickly from the stomach to the small intestines. If the pylorus releases too much food, too quickly, blood glucose levels surge from a ‘gastric dump.’ The stomach has simply allowed too much food to enter the small intestines at once. The blood stream cannot absorb all of this glucose. Glucose levels during a “dumping” can be upwards of 250-300, or even higher. The pancreas receives a signal from the blood stream there is too much glucose to handle. In turn, the pancreas begins secreting a large amount of insulin. Insulin continues to flood the blood stream, trying to take as much as it can to be stored in the liver through Glycogenesis.
Dumping after meals can happen early or late. Early dumping occurs within 30-45 minutes of eating. Late dumping typically occurs 60-90 minutes after eating. No matter the release, PPH results are the same.
You’ll remember that when blood glucose decreases to safe levels once more, the pancreas stops releasing insulin and Glycogenesis comes to a halt. When insulin doesn’t stop, PPH occurs. In PPH, the pancreas continues to release insulin even though blood glucose levels are normal again. As insulin continues to be released, glucose keeps being removed from the blood stream and stored in the liver. As a result, blood glucose drops to unsafe levels. Measurements are often in the 50-60 range. These unsafe levels are referred to as Hypoglycemia.
Causes of Gastric Dumping
Dumping causes are often varied and unknown. Doctors do not know exactly why the body continues releasing insulin after it is medically necessary. They do have some theories to what may contribute to this condition. Illness can be a factor as viruses and bacteria disrupt the normal patterns of digestion. Anatomy anomalies such as malrotations of the intestines and malformed organs can cause abnormal digestive patterns as well. Gastric surgeries often create abnormal pyloric sphincter patterns due to reconstruction or anatomical changes. Disrupted muscle functions and damaged nerves from these surgeries can also contribute to quick chyme release. The nerve most often damaged during gastric surges is the Vagus nerve. The tenth of the cranial nerves, it innervates most thoracic organs and controls many autonomic functions.
Diagnosis
Diagnosing PPH is typically accomplished by measuring blood glucose levels before, during, and after meals. Measurement are often taken 30, 60, 90, and 120 minutes after eating. Graphing the changes can pinpoint early or late dumping. These numbers can also identify when medications should to be taken in relation to meals.
Treatment
Treatment options can either be used to regulate the emptying of the stomach, or to treat the resulting symptoms. Gastroparesis (delayed gastric emptying) medications can help by regulating peristalsis pattern when the stomach ins’t moving regularly. These medication are called prokinetics. Popular prokinetics are metoclopromide (Reglan), domperidone (Motilum), and erythromycin (EryPed). Other helpful medications such as hyoscyamine (Levsin) and bethanechol chloride (Urecholine) help regulate muscle contractions. Nausea and pain medications can help. The most common are ondansetron (Zofran), cyproheptadine (Periactin), and dyphenhydramine (Benadryl). Lifestyle changes such as smaller meals and larger carbohydrate molecule foods like complex carbohydrates can help slow digestion if early dumping occurs.
PPH may improve over time with resolution of illness or anatomical corrections. Surgically induced PPH is often a chronic condition that needs to be managed with lifestyle changes and medication. As always, remember to speak with your gastroenterologist before beginning any medication regimen.
###
Katie is a freelance writer about digestive and nutritional health. She believes accurate and valuable information should be easy to find!
Your email address will not be published. Required fields are marked with *.